Many Privately-Insured Pennsylvanians Receive Unexpected Medical Bills; Fully One-Third Unhappy with Resolution, May Not Understand Options for Assistance
Unexpected medical bills are surprisingly common. These bills can take many forms, from higher-than-expected charges, to bills from unexpected doctors, to bills from out-of-network providers when patients thought they were in-network. Federal and states legislators are taking a close look at these issues and expanding consumer protections to reduce the patient’s financial burden from unexpected medical bills.
A 2018 survey of Pennsylvania adults examined how prevalent surprise bills are in the Commonwealth. While respondents reported receiving unexpected bills regardless of insurance status, this analysis focuses on the respondents with private health insurance, that is insurance from an employer or that you purchase on your own. Compared to adults with Medicare, Medicaid, Tri-care or Veterans Health, consumers with private insurance have fewer protections against high and unexpected out-of-pocket costs.1
Key Findings:
- One in three privately-insured Pennsylvania adults received a surprise medical bill
- Three-quarters of privately-insured Pennsylvanians who received a surprise bill made an effort to resolve the bill before paying it
- More than half paid the bill in full
- Only one quarter of surprise medical bills were resolved satisfactorily
- Many respondents may not realize they have options for appealing these bills
Nearly one in three privately-insured Pennsylvania adults received a medical bill they were not expecting. Altogether, 31% of privately-insured Pennsylvania survey respondents told us they received a medical bill that included an unexpected expense in the prior 12 months. The most common type of unexpected bill was one where the amount charged was higher than expected, followed by bills from an unexpected doctor.
Smaller numbers reported: being charged out-of-network rates when they thought the doctor was in-network; being charged for services they did not receive, or experiencing something else unexpected. The prevalence of unexpected bills aligns well with other surveys of privately-insured adults.2
Pennsylvanians tried a number of strategies to address the surprise bill but were often dissatisfied with the resolution. Fully three-quarters (78%) of privately-insured Pennsylvanians who received a surprise bill made an effort to resolve the bill before paying it. As a first step, 40% contacted their insurance plan and 21% contacted the doctor, hospital or lab to resolve their unexpected medical bill (see Table 1).
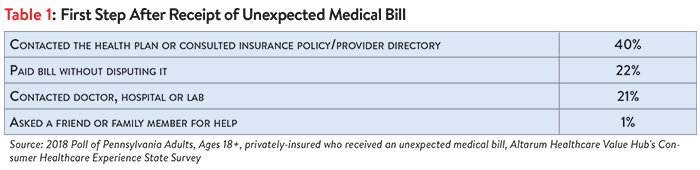
Just 13% of privately-insured Pennsylvania adults took more than one step to resolve the unexpected bill. Very few reported taking actions that would escalate the issue beyond the insurer, doctor or hospital, such as:
- Filing an insurance appeal
- Contacting a state government agency
- Contacting state legislators or member of Congress
- Contacting a lawyer
- Filing a formal complaint
It is likely that many patients may not realize these avenues of appeal are open to them. The survey also asked about respondents’ confidence in the skills needed to navigate the healthcare system. Areas where Pennsylvania adults particularly lacked confidence include disputing medical bills and resolving problems with unresponsive providers and health plans. These findings are consistent with other data showing that many adults have a poor understanding of how to navigate financial aspects of the healthcare system, and lack critical knowledge like knowing they have the right to appeal a coverage decision, how to seek help from state regulators and how to navigate hospital charity care policies.3
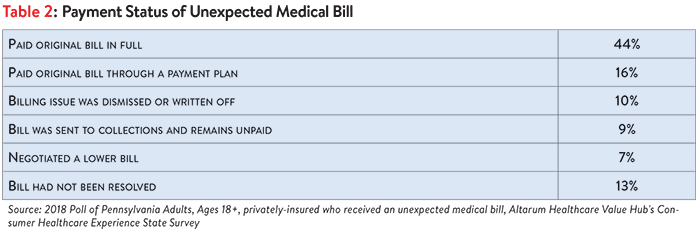
Among privately-insured Pennsylvania adults with an unexpected medical bill in the past 12 months, most paid the bill in full or through a payment plan. Most privately-insured Pennsylvania adults (60%) paid their unexpected bill in full or through a payment plan. Only a small minority were able to negotiate a lower bill or have their bill dismissed (17%) while 9% of privately insured respondents indicated their unexpected medical bill was sent to collections and left unpaid (see Table 2).
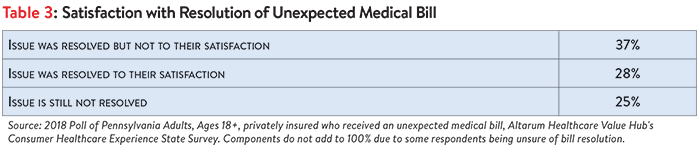
Only one-quarter of unexpected medical bills were resolved satisfactorily; many remain unresolved. Among privately-insured Pennsylvania adults who had an unexpected medical bill, just over one-quarter indicated that the issue was resolved to their satisfaction. More than one-third indicated that the issue was not resolved to their satisfaction. For another 25%, the issue had not been resolved (see Table 3).
Satisfied consumers tended to contact a state government agency more often (9%) than dissatisfied consumers (3%) and were more likely to have either negotiated a lower payment or had their bill written off or dismissed. In contrast, consumers dissatisfied with how their medical bill was resolved more often reported paying their bill without disputing it.
Discussion
Privately-insured Pennsylvania adults receive unexpected medical bills at an alarming rate. These bills take many forms, from higher than expected charges, to bills from doctors they didn’t expect, to surprise out-of-network bills. Distressingly, more than one-third of these unexpected bills are not resolved to the satisfaction of the recipient and many more remain unresolved.
Data showing that survey respondents “tried to do the right thing,” with three-quarters making an initial effort to resolve the unexpected bill by contacting the doctor, hospital or health plan. Very few respondents escalated their concerns to formal appeal channels. This may signal that consumers are unfamiliar with their right of appeal, how to seek help from state regulators or how to navigate hospital charity care policies.4
Pennsylvania residents would benefit significantly from state actions to alleviate these unfair and burdensome medical billing problems, starting with protections that prevent unexpected bills from happening in the first place.
As states address the issue of surprise medical bills related to out-of-network care, they are emphasizing the need to get the consumer out of the middle—strategies such as better consumer notices and prohibiting balance billing by providers in certain circumstances.5 When balance billing is prohibited, these consumer protections must be accompanied by a mechanism to resolve the out-of-network provider’s bill.
Other efforts states are undertaking include simplifying health plan benefit designs6 and improving the accuracy of provider directories and adequacy of provider networks. In light of poll results showing that few bill recipients take more than one step to resolve their bill, Pennsylvania policymakers may also want to consider creating a dedicated state ombudsman’s office to help consumers with their billing problems, such as available in Connecticut and Vermont.7
Notes
1. Medicaid and Medicare have basic prohibitions against “balance billing.”
2. A 2018 Consumer Reports survey found that nearly one-third of privately-insured Americans were hit with surprise medical bills. https://www.consumerreports.org/medical-billing/sick-of-confusing-medical-bills/ In addition, a Kaiser Family Foundation survey finds that among insured, non-elderly adults struggling with medical bill problems, charges from out-of-network providers were a contributing factor about one-third of the time. A study by Yale University found 22% of visits to emergency departments resulted in surprise medical bills.
3. A 2014 Kaiser Family Foundation survey found one-third of respondents did not know that if a health plan refuses to pay for a medically recommended service, an insured person has the right to appeal the plan’s decision. https://www.kff.org/health-reform/poll-finding/assessing-americans-familiarity-with-health-insurance-terms-and-concepts/. A separate 2015 survey found three-quarters of privately insured adults are unsure if they have the further right to appeal to the state/an independent medical expert if their health plan refuses coverage for medical services they think they need. Few (just 13%) could identify the state agency/department tasked with handling health insurance complaints. https://consumersunion.org/research/surprise-bills-survey/
5. Lucia, Kevin, Jack Hoadley, and Ashley Williams, Balance Billing by Health Care Providers: Assessing Consumer Protections Across States, CommonwealthFund (June 13, 2017).
6. For examples, see Corlette, et. al., Missed Opportunities: State-Based Marketplaces Fail to Meet Stated Policy Goals of Standardized Benefit Designs, Urban Institute (July 2016).
7. Hunt, Amanda, The Office of the Healthcare Advocate: Giving Consumers a Seat at the Table, Healthcare Value Hub, Research Brief No. 25 (May 2018).
Methodology
Altarum’s Consumer Healthcare Experience State Survey (CHESS) is designed to elicit respondents’ unbiased views on a wide range of health system issues, including confidence using the health system, financial burden and views on fixes that might be needed.
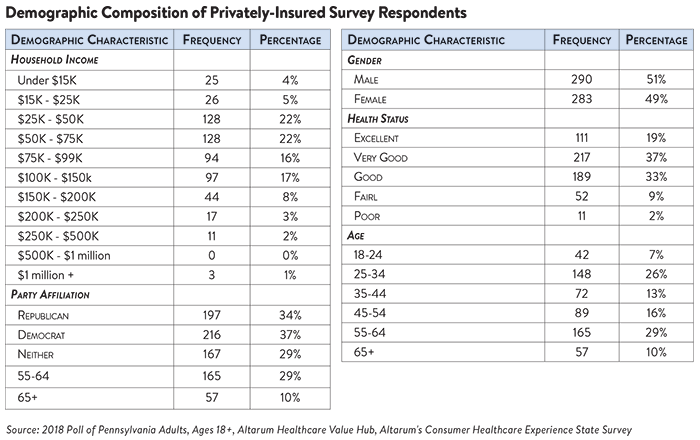
The survey used a web panel from SSI Research Now with a demographically balanced sample of approximately 1,000 respondents who live in Pennsylvania. The survey was conducted only in English and restricted to adults ages 18 and older. Respondents who finished the survey in less than half the median time were excluded from the final sample. Moreover, for purposes of this data brief, we restricted the analysis to only those with private insurance (through respondent’s employer or purchased on their own) leaving 580 cases for analysis. After those exclusions, the demographic composition of privately-insured respondents was as follows: