North Carolina Survey Respondents Bear Health Care Affordability Burdens Unequally; Distrust of/Disrespect by Health Care Providers Leads Some to Delay/Go Without Needed Care
Key Findings
A survey of more than 1,400 North Carolina adults, conducted from October 18 to October 23, 2023,
found that:
- Nearly seven out of ten (68%) North Carolina respondents have experienced one or more health care affordability burdens in the past 12 months. Over four in five (85%) worry about affording some aspect of health care now or in the future.
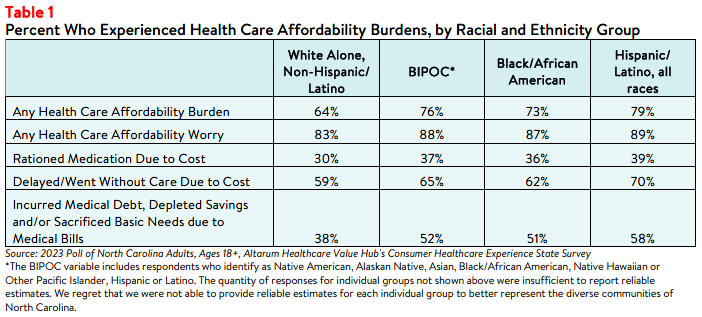
- Respondents of color experienced greater affordability burdens than their white alone, non-
- Hispanic counterparts: 76% of respondents of color have experienced one or more health care affordability burdens in the past 12 months, including 79% of Hispanic/Latino respondents, compared to 64% of white alone, non-Hispanic respondents.
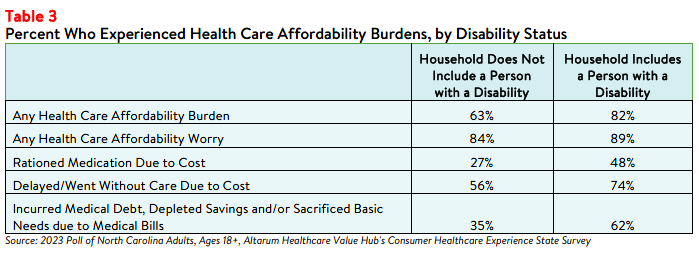
- Respondents living in households with a person with a disability more frequently reported affordability burdens than respondents without a disabled household member, including rationing medication due to cost (48% versus 27%); delaying or going without care due to cost (74% versus 56%); and going into medical debt, depleting savings or sacrificing basic needs due to medical bills (62% versus 35%).
- Thirty-one percent of respondents of color skipped needed medical care due to distrust of or feeling disrespected by health care providers, compared to 15% of white alone, non-Hispanic respondents.
- Sixty-one percent of all respondents think that people are treated unfairly based on their race or ethnic background somewhat or very often in the U.S. health care system.
Differences in Affordability Burdens & Concerns
Race
The intersection of racial disparities in health care and affordability issues impact access to care and may
contribute to financial burdens for communities of color, particularly Black and Hispanic/Latino
communities.1,2 In North Carolina, respondents of color reported higher rates of affordability burdens than
white alone, non-Hispanic/Latino respondents, including incurring medical debt, depleting savings, or
sacrificing basic needs (like food, heat and housing) due to medical bills (see Table 1).
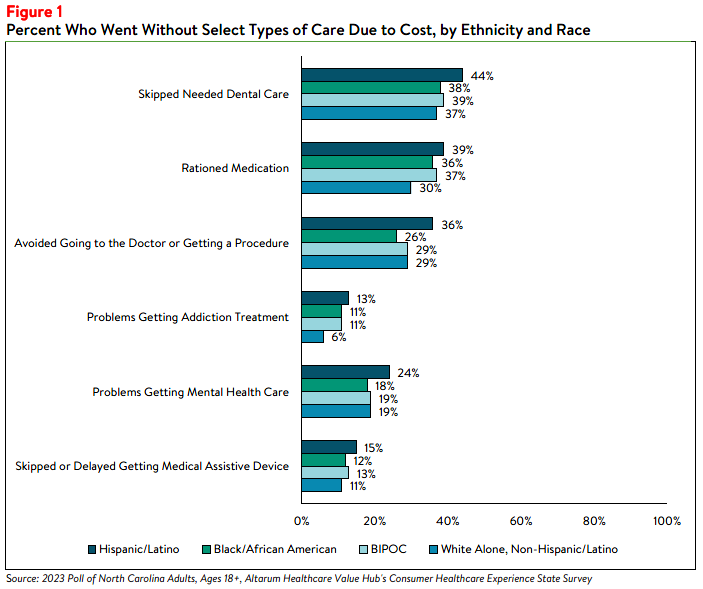
In addition to incurring medical debt, respondents of color more frequently reported difficulty getting
select types of care compared to white, non-Hispanic respondents in all but two categories. For example,
Hispanic/Latino respondents most frequently reported challenges accessing mental health care and
addiction treatment, as well as avoiding going to the doctor or getting a procedure done due to cost (see
Figure 1).3
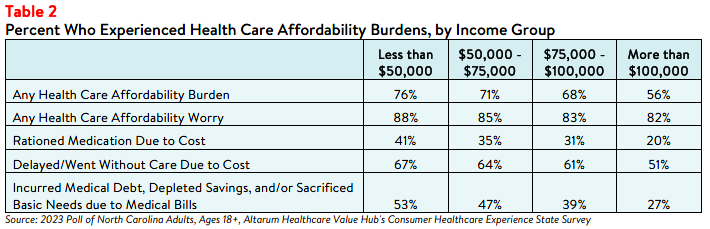
Income
The survey also revealed differences in how North Carolina respondents experience health care
affordability burdens by income. Unsurprisingly, respondents at the lowest end of the income spectrum
most frequently reported affordability burdens, with over three-fourths (76%) of those with household
incomes less than $50,000 per year struggling to afford health care in the past 12 months (see Table 2).
Still, over half of respondents living in middle- and high-income households also reported struggling to
afford some aspect of coverage or care, demonstrating that affordability burdens impact people all income
groups. Likewise, at least 85% of respondents in each income group reported being worried about
affording health care either now or in the future.
Additionally, two-fifths (41%) of respondents with household incomes of $50,000 or less reported not
filling a prescription, skipping doses of medicines, or cutting pills in half due to cost. Lower- and middle-
income respondents also most frequently reported financial consequences after receiving health care
services—53% of respondents who earned less than $50,000 per year and 47% of respondents who earned between $50,000 and $75,000 a year either went into medical debt, depleted their savings, or sacrificed other basic needs (like food, heat, or housing) due to medical bills.
Disability Status
People with disabilities interact with the health care system more often than those without disabilities and,
as a result, tend to face more out-of-pocket costs.4 Additionally, people who receive disability benefits
face unique coverage challenges that impact their ability to afford needed care, such as the possibility of
losing coverage if their household income or assets increase over a certain amount (for example, after
getting married).5 North Carolina respondents who have or live with a person who has a disability more
frequently reported a diverse array of affordability burdens compared to others (see Table 3). These
respondents also more frequently reported worrying about future health care affordability in general (89%
versus 84%) and losing health insurance specifically (46% versus 25%).
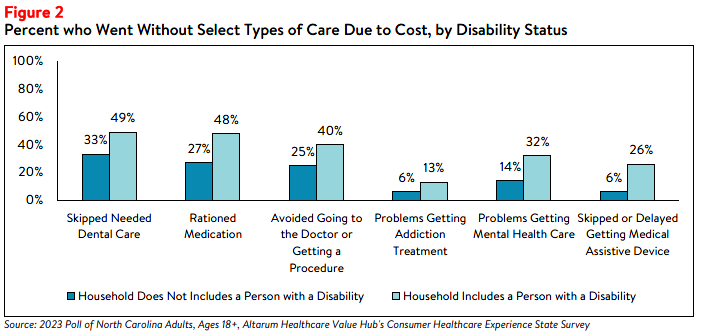
Those with disabilities also face health care affordability burdens unique to their disabilities—26% of
respondents reporting a disability in their household delayed getting a medical assistive device such as a
wheelchair, cane/walker, hearing aid or prosthetic limb due to cost. Just 6% of respondents without a
disability (who may have needed such tools temporarily or may not identify as having a disability) reported
this experience (see Figure 2). Similarly, 32% of respondents reporting a disability in their household
reported problems getting mental health care compared to 14% of households without a person with a
disability.
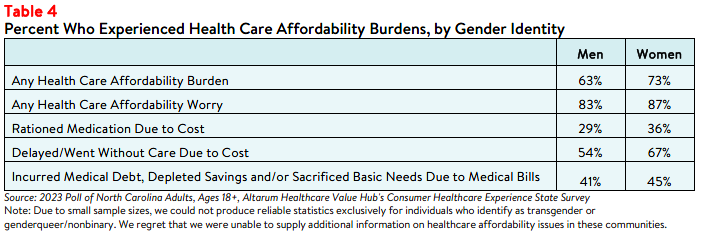
Gender
The survey also surfaced differences in health care affordability burdens and worry by gender. Women who responded to the survey reported higher rates of experiencing at least one affordability burden in the past year than those identifying as men (73% versus 63%) (see Table 4). Women also more frequently reported delaying or going without care due to cost in general and reported higher rates of rationing their
medications by not filling a prescription, skipping doses, or cutting pills in half. While many respondents
regardless of gender reported being somewhat or very concerned about health care costs, a higher
percentage of women reported worrying about affording some aspect of coverage or care than men (87%
versus 83%).
Due to the small sample size, this survey could not produce reliable estimates exclusively for transgender,
genderqueer, or nonbinary respondents. However, it is important to note that these groups experience
unique health care affordability burdens—24 (1% of) survey respondents reported that they or a family
member had trouble affording the cost of gender-affirming care, such as hormone therapy or
reconstructive surgery.
Distrust and Mistrust in the Health System
Whether a patient trusts and/or feels respected by their health care provider may impact whether they
seek needed care. In North Carolina, just over 3 in 10 (31% of) respondents reported that their provider
never, rarely, or only sometimes treats them with respect. When asked why they felt health care providers
did not treat them with respect, almost half of these respondents cited their income or financial status
(48%), followed by race (27%), disability (24%), ethnic background (20%), and gender/gender identity
(17%). In lesser numbers, respondents cited experience with violence or abuse (7%) and sexual orientation (7%) as reasons for the disrespect.
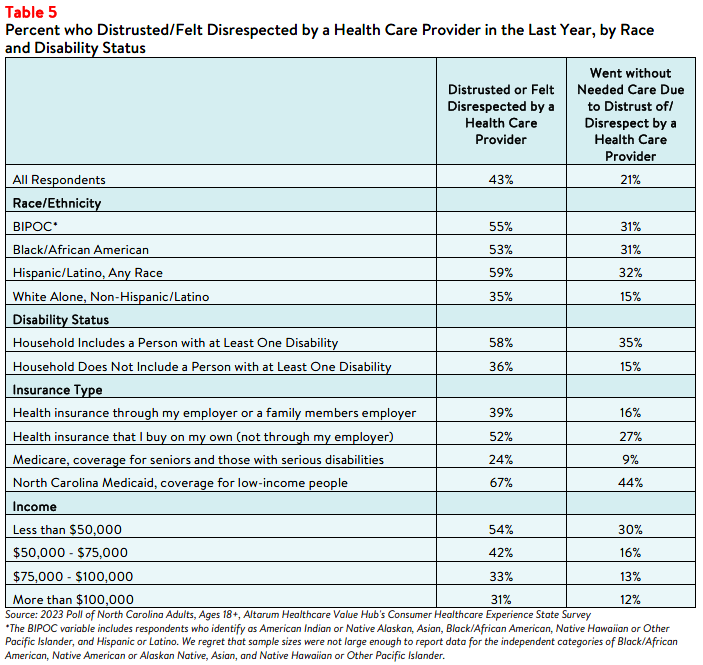
Respondents of color and those with a person with a disability in their household more frequently reported
distrust in and feeling disrespected by their health care providers compared to white respondents and
respondents without a disabled household member (see Table 5). They also more frequently went without
medical care due to that distrust and/or disrespect.
Overall, 21% of respondents of color reported going without needed medical care due to distrust of or
feeling disrespected by health care providers, including 32% of Hispanic/Latino respondents, compared to
only 15% of white, non-Hispanic respondents. Additionally, 35% of respondents who have or are living with a person with a disability went without care due to distrust or disrespect, compared to 15% of those
without a household member with a disability.
Respondents with North Carolina Medicaid coverage reported the highest rates of distrusting or feeling
disrespected by a health care provider compared to respondents with other insurance types. In addition,
respondents earning less than $50,000 most frequently reported distrust/disrespect and going without
care due to distrust/disrespect, although middle- and high-income earners also reported this issue.
Individual & Systemic Racism
Respondents perceived that both individual and systemic racism exist in the U.S. health care system. Sixty-one percent of respondents believe that people are treated unfairly based on their race or ethnic
background, either somewhat or very often. When asked what they think causes healthcare systems to
treat people unfairly based on their race or ethnic background:
- 1 in 5 (21%) cited policies and practices built into the health care system;
- 1 in 10 (10%) cited the actions and beliefs of individual health care providers; and
- Over 2 out of 5 (46%) believe it is an equal mixture of both.
Disatisfaction with the Health System and Support for Change
Given this information, it is not surprising that 75% of North Carolina respondents agree or strongly agree
that the U.S. health care system needs to change. Understanding how the health care system
disproportionately harms some groups of people over others is key to creating a fairer and higher value
system for all.
Making health care affordable for all residents is an area ripe for policymaker intervention, with widespread support for government-led solutions across party lines. For more information on the types of strategies North Carolina residents want their policymakers to pursue, see: North Carolina Residents Struggle to Afford High Healthcare Costs; Worry about Affording Healthcare in the Future; Support Government Action across Party Lines, Healthcare Value Hub (December 2023).
Notes
- Fadeyi-Jones, Tomi, et al., High Prescription Drug Prices Perpetuate Systemic Racism. We Can Change It, Patients forAffordable Drugs Now (December 2020), https://patientsforaffordabledrugsnow.org/2020/12/14/drug-pricing-systemic-racism/
- Kaplan, Alan and O’Neill, Daniel, “Hospital Price Discrimination Is Deepening Racial Health Inequity,” New England Journal of Medicine—Catalyst (December 2020), https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0593
- A small share of respondents also reported barriers to care that were unique to their ethnic or cultural backgrounds. Two percent reported not getting needed medical care because they couldn’t find a doctor of the same race, ethnicity or cultural background as them and <1% percent because they couldn’t find a doctor who spoke their language.
- Miles, Angel L., Challenges and Opportunities in Quality Affordable Health Care Coverage for People with Disabilities, Protect Our Care Illinois (February 2021), https://protectourcareil.org/index.php/2021/02/26/challenges-and-opportunities-in-quality-affordable-health-care-coverage-for-people-with-disabilities/
- A 2019 Commonwealth Fund report noted that people with disabilities risk losing their benefits if they make more than $1,000 per month. According to the Center for American Progress, in most states, people who receive Supplemental Security are automatically eligible for Medicaid. Therefore, if they lose their disability benefits they may also lose their Medicaid coverage. Forbes has also reported on marriage penalties for people with disabilities, including fears about losing health insurance. See: Seervai, Shanoor, Shah, Arnav, and Shah, Tanya, “The Challenges of Living with a Disability in America, and How Serious Illness Can Add to Them,” Commonwealth Fund (April 2019), https://www.commonwealthfund.org/publications/fund-reports/2019/apr/challenges-living-disability-america-and-how-serious-illness-can; Fremstaf, Shawn and Valles, Rebecca, “The Facts on Social Security Disability Insurance and Supplemental Security Income for Workers with Disabilities,” Center for American Progress (May 2013),
https://www.americanprogress.org/article/the-facts-on-social-security-disability-insurance-and-supplemental-security-income-for-workers-with-disabilities/; and Pulrang, Andrew, “A Simple Fix For One Of Disabled People’s Most Persistent, Pointless Injustices,” Forbes (April 2020), https://www.forbes.com/sites/andrewpulrang/2020/08/31/a-simple-fix-for-one-of-disabled-peoples-most-persistent-pointless-injustices/?sh=6bfab1a26b71
Methodology
Altarum’s Consumer Healthcare Experience State Survey (CHESS) is designed to elicit respondents’ unbiased views on a wide range of health system issues, including confidence using the health system, financial burden, and views on fixes that might be needed.
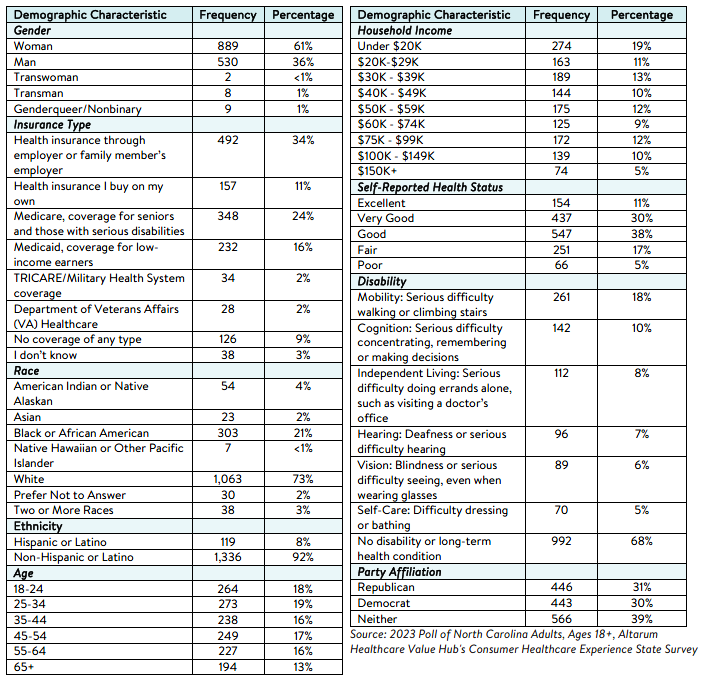
This survey, conducted from October 18 to October 23, 2023, used a web panel from online survey company Dynata with a demographically balanced sample of approximately 1,500 respondents who live in North Carolina. Information about Dynata’s recruitment and compensation methods can be found here. The survey was conducted in English or Spanish and restricted to adults ages 18 and older. Respondents who finished the survey in less than half the median time were excluded from the finalsample, leaving 1,455 cases for analysis. After those exclusions, the demographic composition of respondents was as follows, although not all demographic information has complete response rates:
based on organizational/advocacy priorities. We do not report any estimates under N=100 and a co-efficient of variance more than 0.30