Improving Value
Medical Homes
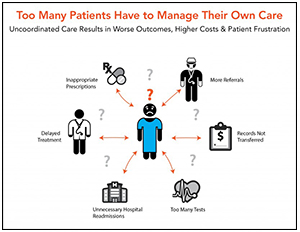
Patient-Centered Medical Homes (PCMHs) aim to deliver efficient, patient-centered primary care. Specifically, PCMHs strive to provide patients with what they say they want in healthcare - having a personal relationship with their doctor; feeling valued; being treated as a whole person and not just a series of illnesses; having adequate time to talk to the doctor and not feeling rushed; and good bedside manner and listening skills.1
While most experts support the goal of PCMHs, there are varying views on the characteristics of a "good" PCMH, how the transformation should occur and how results should be measured. Because there is no single definition for a PMCH and no one organization responsible for recognizing, accrediting and/or defining the model,2 PCMHs may look different while attempting to achieve similar goals. More research is needed to determine the most effective PCMH models, the best way to transition from traditional practice into a PCMH and to improve our methods for measuring the consumer experience.
Notes
1. For example, see Quincy and Kleimann, "Engaging Consumers on Healthcare Cost and Value Issues," Consumers Union (October 2014); "Talking about Healthcare Payment Reform with U.S. Consumers: Key Communications Findings from Focus Groups," Robert Wood Johnson Foundation (April 2011); and Schleifer, David, et al., "Curbing Health-Care Costs: Are Citizens Ready to Wrestle with Tough Choices?," Public Agenda and Kettering Foundation (2014).
2. Klein, David B., et al., "The Patient-Centered Medical Home: A Future Standard for American Healthcare?," Public Administration Review (April 2013).
- AHRQ: Patient Center Medical Home Resource Center (Feb. 11, 2019).
- NCQA: Patient Centered Medical Home
- Journal of General Internal Medicine: Defining and Measuring the Patient-Centered Medical Home (May 2010).