Improving Value
Better Coordinated Care for Complex Cases
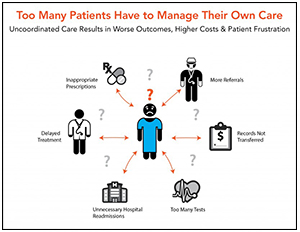
"Complex" patients represent a minority of the general population but drive a significant portion of healthcare spending. Estimates suggest that the costliest one percent of patients account for 20 percent of healthcare spending, while the costliest five percent of patients drive 50 percent. Many of these patients have multiple chronic conditions that require treatment from different providers. These providers don't always communicate with one another, however, which can sacrifice health outcomes, increase costs and frustrate patients.
Care coordination programs that treat patients holistically have emerged as an important strategy to deliver care efficiently and reduce unnecessary costs. Some programs integrate medical care with dental, behavioral and/or home health services, while others go even further to incorporate efforts to address social determinants of health, like access to transportation, adequate housing or healthy food. Social-medical models, in particular, have been shown to improve health outcomes, as approximately 40 percent of health outcomes are determined by social and economic factors.
The diversity of care coordination programs prevents researchers from conducting rigorous side-by-side comparisons to evaluate overall effectiveness. Individual evaluations show that some programs have achieved their goal to deliver high quality care, while others have attained mixed results. Nevertheless, analysis of successful models reveals some common themes:
- Effective care coordination programs are highly targeted, meaning that care teams use evidence-based criteria to determine which patients are most likely to benefit. Ofte, this involved a comprehensive assessment of patients' medical, functional, social and behavioral needs.1
- Effective care coordination requires an efficient informaiton exchange. All participants in a patient's interdisciplinary care team must be able to access up-to-date and comprehensive information in a timely manner. This requirement not only applies to the use of electronic record keeping systems, but also extends to relationships between team members.
- Effective programs must also use trained care coordinators. These professionals serve as the glue for the interdisciplinary care team, facilitating coordination and communication between the patient and the interdisciplinary care team. Like other members of the team, care coordinators' roles and responsibilities should be clearly defined. They can be nurses, social workers, community health workers or patient navigators by trade, but they should also be experts on local resources and the factors contributing to health disparities within their communities.
- Successful programs consistently evaluate performance to monitor progress. Tracking quality measures related to patient experience, health outcomes, process improvement, community and population health and cost savings allows care teams to quantify positive impact and identify areas for improvement.2
Financial incentives are also important when it comes to incentivizing providers to work together to deliver better care. More information on provider payment reform can be found here.
Notes
1. National Academy of Medicine, "Effective Care for High Need Patients: Opportunities for Improving Outcomes, Value, and Health," Washington, D.C. (2017).
2. Alfero, Charles, et al., "Care Coordination in Rural Communities: Supporting the High Performance Rural Health System," Rural Policy Research Institute, Iowa City, Iowa (June 2015).
- RAND Corporation: Identifying and Coordinating Care for Complex Patients: Findings from the Leading Edge of Analytics and Health Information Technology (June 2017).
- Agency for Healthcare Research and Quality: Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination) (June 2007).
- American Journal of Managed Care: Multi-Payer Advanced Primary Care Practice Demonstration on Quality of Care (September 2019).