Cost & Quality Problems
Too Much Waste in Our Health Care System
There are a variety of estimates on how much of our health care spending is “wasteful,” but there is general consensus that it is far too large a share of our spending. Estimates of waste fall between 15 and 30 percent of spending;1 however, research is divided on how much waste can realistically be minimized or eliminated without negatively impacting consumers’ health.
Types of Waste: Administrative, Clinical and Operational
There is no single standard for measuring waste; one common way to look at waste is using the six broad categories identified by the Institute of Medicine: unnecessary services, excess administrative costs, inefficient care delivery, inflated prices, fraud and prevention failures.2
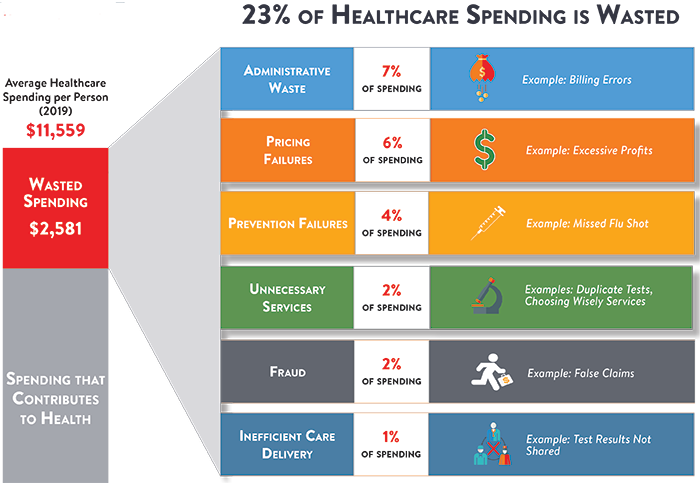
Unnecessary services, including over treatment and over prescription of medication, are the largest category, estimated to account for $210 billion in waste each year. This includes services that lack evidence that they produce better health outcomes compared to less-expensive alternatives.
The provision of unnecessary services seems to be more prevalent in some geographic areas and is not associated with better patient outcomes or significant changes in consumer satisfaction.3,4 For example, high spending areas were found to provide Medicare patients with as much as 60 percent more care compared to the lowest spending areas; however, few quality scores improved as a result of the increased spending.5,6 Studies surrounding unnecessary services primarily focus on antibiotics and cardiovascular procedures with serious gaps in research relating to preventive diagnostic services and few newer, more costly procedures.7
Administrative waste is the second largest category and is accumulated through excessive administration costs and profits, including claims processing, ineffective use of IT, staffing turnover and paper prescriptions. These costs are approximately $130 billion per year.8,9 In part, administrative waste stems from our fragmented way of paying for health care. But even without changing the way we pay for care, experts estimate we could eliminate a percentage of administrative spending without reducing access to care. A recent focus on improving the processing of claims has driven down the error rate and response time and increased cost savings, however, avoidable errors and inefficiencies in the claims process alone still added an average of $2.36 to every insurance claim in 2013.10
Inefficient care delivery, when doctors don’t effectively ‘talk’ to each other, results in $130 billion in wasteful spending every year. As a result of inefficient care delivery systems, patients receive repetitive tests and/or health complications, reduced functional capacities and often require further medical care in the future. A lack of coordinated care and inefficient IT systems prevent the streamlined delivery of care, and must be addressed in order to provide more consistent care, patient convenience, improved health outcomes and to lower costs.
Inflated unit prices exist as a result of provider market power, product manufacturer market power, non-transparent pricing and our third party system for paying for care. Excess prices account for $105 billion in wasteful spending every year and durable medical equipment alone is estimated to be inflated by at least 20 percent.11 Medications, however, are a much more complicated market that depends on patent exclusivity, the availability of a generic and the dispensing process.
While hard to pin down, between $75-272 billion of wasteful spending in the U.S. can be attributed to fraud and abuse, billed services that produce no value for our system.
The final category of waste, prevention failures, refers to treatments or services provided to consumers with conditions that could have been prevented in a much more affordable fashion and accounts for $55 billion of wasteful spending and a very human cost when it results in periods of poor health. For example, missed vaccinations, or failure to monitor and treat chronic conditions like diabetes may result in serious and costly health complications, decreased functionality and increased dependency of patients on costly health services. These costs include services to support consumers with chronic conditions, obesity, smoking, non-adherence and alcoholism.
Why Clinical Waste Occurs
According to physicians, “aggressive” practice styles of providing excessive or unnecessary care results from a variety of factors including practicing defensive medicine to mitigate malpractice concerns, generating revenue, patient demand and limited patient interaction time to more appropriately triage a health complaint without tests or services.
Clinical performance measures and financial incentives such as increased reimbursement for high patient satisfaction scores, although an effective tool to increase patient satisfaction, may also encourage overtreatment. In some cases, these incentives may drive physicians to comply with patient requests despite a clear lack of efficiency.12
With the average patient appointment lasting less than 20 minutes, providers feel great pressure to deliver care that is fast, efficient and to address any patient demands.13,14 These pressures make it difficult to allocate a sufficient portion of the limited appointment time to discuss costs associated with the treatment and more efficient alternatives.15
Additionally, income generation may act as an incentive for some providers to overutilize health services. Thirty-nine percent of physicians believe other physicians “aggressively” order diagnostic tests to generate extra income.16
Strategies to Address Waste
By definition, waste is health care spending that can be eliminated without reducing the quality of care. While indirect evidence suggests a massive amount of waste exists in the U.S. health care system, it is much harder to identify the specific procedures and activities that can be eliminated, in part because some procedures identified as commonly overused may nonetheless benefit some consumers. An angioplasty inserting coronary stents, for example, is considered one of the most overused medical interventions in the U.S. However, some doctors argue that only a small portion of the procedures have questionable medical necessity.17 As a result, policy makers proposing cost containment measures will walk a fine line between eliminating “true” waste while not establishing barriers to patients seeking legitimate care.
A myriad of reforms can help identify and reduce the waste we pay for in the U.S. health care system. For example, policies should focus on:
-
Filling in our gaps in comparative effectiveness research and effectively implement best patient practices.
-
Implementing transparency initiatives to decrease inflated unit prices.
-
Introducing payment reform including:
-
Strong financial incentives to reduced medical harm, such as reduced hospital readmissions through care coordination and Medicare penalties.
-
Bundled payments and pay for performance that incent reducing waste while still providing provider latitude to recommend generally ineffective treatments if clinically indicated.
-
Financial incentives and techniques for shared decision making to bring informed patient preferences into the picture.
-
Malpractice reform.
-
-
Addressing fraud and abuse
Challenges to eliminating waste includes include barriers such as difficulty of culture change, or the lack of agility or willingness to make processes “right” instead of easy, political conflicts, lack of alignment with financial incentives and lack of a coordinated care focus.18
Notes
1. Delaune, Jules, and Wendy Everett, "Waste and Inefficiency in the U.S. Healthcare System," New England Healthcare Institute, Cambridge, M.A. (February 2008).
2. Pierre L., and Leigh Anne Olsen, "The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary," Institute of Medicine, 2010.
3. Alberti, Mike, “Keeping the “best care” option out of the health spending equation,” Remapping Debate, (Feb. 27, 2013).
4. Kale, Minal S., et al., "’Top 5’ Lists Top $5 Billion.” Archives Of Internal Medicine, Vol. 171, No. 20 (October 2011).
5. Fisher, Elliott S., et al., “The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care. Annals of Internal Medicine,” Annals of Internnal Medicine, Vol. 138, No. 4 (Februuary 2013).
6. Pierre L., and Leigh Anne Olsen, "The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary," Institute of Medicine, 2010.
7. Korenstein, Deborah, et al., “Overuse of Healthcare Services in the United States an Understudied Problem,” JAMA,Vol. 172, No. 2 (January 2012).
8. PricewaterhouseCoopers’ Health Research Institute, "The Price of Excess: Identifying waste in healthcare spending," Cambridge, M.A. (2010).
9. Berwick, Donald M., and Andrew D. Hackbarth, "Eliminating Waste in U.S. Healthcare," JAMA, Vol. 307, No. 14 (March 2012).
10. American Medical Association, "2013 National Health Insurance Report Card," (2013).
11. Pierre L., and Leigh Anne Olsen, "The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary," Institute of Medicine, 2010.
12. Fenton, Joshua J., et al. “The cost of satisfaction: a national study of patient satisfaction, healthcare utilization, expenditures, and mortality,” Archives Of Internal Medicine, Vol. 172, No. 5 (March 2012).
13. Cherry, Donald K., and David A. Woodwell, "National Ambulatory Medical Care Survey: 2000 Summary. Advanced Data, From Vital and Health Statistics," National Center for Health Statistics, Hyattsville, M.D. (2002).
14. Schoen, Cathy, Collins, Karen S., and Davod R. Sandman, "The Commonwealth Fund Survey of Physician Experiences with Managed Care," The Commonwealth Fund, New York, N.Y., (March 1997).
15. PerryUndem Research/Communication, "Unnecessary Tests and Procedures In the Healthcare System," Robert Wood Johnson Foundation and ABIM Foundation, (May 2014).
16. Sirovich, Brenda E., Woloshin, Steven, and Lisa M. Schwartz,“Too Little? Too Much? Primary care physicians' views on US healthcare: a brief report. Archives Of Internal Medicine” JAMA, Vol. 171, No. 17, (September 2011).
17. Alberti, Mike, “Keeping the “best care” option out of the health spending equation,” Remapping Debate, (Feb. 27, 2013).
18. PricewaterhouseCoopers’ Health Research Institute, "The Price of Excess: Identifying waste in healthcare spending," Cambridge, M.A. (2010).






