Consumer-Focused Health System Transformation: What are the Policy Priorities?
A Policy Roadmap and Toolkit
The U.S. healthcare system is transforming in response to many types of pressures. To ensure these changes benefit the people the system is intended to serve, policymakers, funders, advocates and others need actionable information to guide improvement efforts. Moreover, given the complexity of the health system, it is imperative that these efforts are systematic and evidence-based.
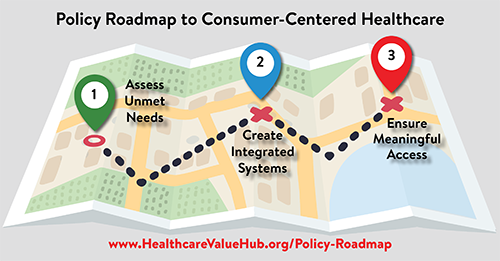
The following policy compendium serves as a roadmap—highlighting a promising set of federal, state and (occasionally) local policies to achieve our health system transformation goal:
Ensuring that the healthcare system works seamlessly with public health, social sectors and community members to address the goals and needs of the people it serves and advance health equity.
Our work relied heavily on informal interviews with experts from a wide variety of policy fields. The conversations yielded three “interim destinations” on the road to achieving our transformation goal:
-
Assess people’s physical, behavioral and oral health, as well as social needs, and identify gaps in the community’s capacity to address them;
-
Create integrated systems to advance population health; and
-
Ensure meaningful access to care and services that meet people’s goals and needs, especially within underserved communities.
Key Themes
Themes that repeatedly surfaced from our discussions with key experts include:
- Strong measurement systems are needed to know where we are headed and whether or not our changes are working. Our experts stressed that collectively agreed upon measures of success must be established to determine if policies are effective. Similarly, “feedback loops” at many levels are essential to ensuring that people’s health-related goals and needs are addressed. Finally, performance measures for providers should be aligned with performance goals for the overall health system, in addition to broader measures used to gauge progress towards community goals (across heath, social and public health sectors).
- Meeting people’s goals and needs cannot be achieved with a one-size-fits-all approach. Consumers are diverse and interventions must be targeted in a way that allows all people to achieve optimal levels of health and well-being.
- Flexible financing is needed to move healthcare dollars “upstream,” with the caveat that new dollars must also be invested in social sectors, which are severely under-funded.
- Primary care, dental care, behavioral healthcare and social services should be integrated, and ideally co-located, to improve patient convenience and outcomes. Successful integration will require aligned incentives, interoperable data systems that share patient information and empowered care coordinators for patients with complex needs.
- States or the Federal government must adopt one of several proven methods to achieve universal coverage to provide access to these improved, integrated systems of care.
Most importantly, across our literature review and our conversations with experts, we found no barrier that was insurmountable to achieving our health transformation goal. Indeed, the Policy Roadmap is replete with proof-of-concept examples of where these policies are already working to make our health system more patient-centered.
A comprehensive set of appendices forms a “toolkit” to make this roadmap easy to use for a variety of audiences:
- Appendix A: Policy Roadmap Summary
- Appendix B: Glossary of Terms
- Appendix C: Key Resources
- Appendix D: Key Federal Policies
- Appendix E: Key State Policies
- Appendix F: Crafting a Roadmap for Your Community: A Checklist
- Appendix G: 10 Places to Start