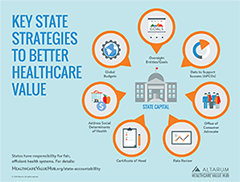
State Strategies to Better Healthcare Value
States play a critical role in how their health systems function, but too few take a coordinated, systematic approach to ensuring that consumers get value for the money they spend. The following sections introduce a number of strategies that states can use to improve healthcare value. Not only do these strategies benefit consumers and employers, but they may (directly or indirectly) alleviate pressure on state budgets, as well.
|
|
Oversight Entities/Goals All states regulate parts of their healthcare systems, but delivering better value requires a comprehensive, inter-agency, multi-payer approach. Despite the critical nature of this function, few states have a centralized oversight agency that focuses comprehensively on reducing healthcare costs, improving quality, bringing spending in line with overall economic growth and implementing new innovations for better value. Our environmental scan of seven state oversight entities revealed striking variation in the responsibilities and powers these entities hold. |
|
|
Data to Support Success (All-Payer Claims Databases) All-payer claims databases (APCDs) are an important tool for understanding healthcare prices, quality and utilization levels within states and measuring progress over time. This brief assesses the ability of APCDs to address unwarranted price variation, healthcare waste and other consumer harms; identifies limitations; and provides best practice suggestions. |
||
|
Office of Consumer Advocate While most states offer some form of assistance to help consumers navigate the health coverage landscape, efforts are often fragmented, with different resources available to consumers depending on their coverage type. Lack of a one-stop-shop can make finding help difficult – many consumers are unaware that help exists or don’t know how to access it. However, a few states have taken a more comprehensive approach. State-established consumer advocacy offices simplify the equation by providing assistance to all healthcare consumers, regardless of coverage type. To maximize impact, they also advocate for better policies to prevent pervasive problems from perpetuating. This research brief profiles high-performing consumer advocacy offices and offers best practices for states looking to increase protections and strengthen representation for consumers. |
||
| |
Rate Review Rate review is the annual process by which state insurance regulators review commercial insurers’ proposed premiums to ensure they are based on (1) accurate, verifiable data and (2) realistic projections of healthcare costs and utilization. This research brief explains how rate review can slow rising health insurance costs, while the accompanying chart highlights states with expanded authority. |
|
 |
Antitrust Laws Competition in healthcare helps keep prices in check, encourages the delivery of high quality products and services and promotes consumer choice. State and federal antitrust laws preserve the benefits of competition in healthcare markets by prohibiting certain anticompetitive behaviors. |
|
|
Certificate of Need Certificate of need (CON) regulations require healthcare providers—primarily hospitals—to demonstrate to a public body the clinical need for a capital expense, such as a new building or major piece of equipment, prior to making an investment. As such, they have long been viewed as a potential cost control solution for states. This Easy Explainer reviews the evidence on CON as a strategy to limit unnecessary spending and address oversupply. |
||
| |
Address Social Determinants of Health As healthcare payers (for Medicaid enrollees, state employees and the incarcerated), states are one of the best stakeholders to invest in and realize the benefits from addressing social determinants of health. Integrating medical and social services is particularly beneficial to state Medicaid programs, where large healthcare expenditures may be driven by low-income patients’ unmet social needs. Addressing these needs not only has the potential to create healthier, more productive populations, but may generate significant savings, as well. The Hub’s inventory of social-medical models highlights current cross-sector partnerships addressing patients’ medical and social needs, many of which target states’ Medicaid populations. |
|
| |
Global Budgets Global budgets are an alternative payment model in which providers–typically hospitals–are paid a prospectively-set, fixed amount for the total number of inpatient, outpatient and emergency services provided annually. Hospitals are responsible for expenditures in excess of the set amount as well as quality outcomes, thus creating an incentive to reduce unnecessary utilization and invest in prevention. Maryland has incorporated global budgets into its long-running all-payer rate setting program, with notable success. Other states, like Pennsylvania, are now testing the utility of the model in a non-rate setting environment. |
|
 |
Expand Scope of Practice Provider scope of practice regulations define the breadth of services a given type of healthcare professional can provide based on their level of education, training and experience. In some states, scope of practice laws limit the extent to which physicians (traditionally the “leaders” of a healthcare team) can delegate tasks to non-physician clinicians who are trained to provide the service, potentially at a lower cost. This brief explores how relaxing regulatory barriers facing non-physician practitioners has the potential to significantly increase access to providers, improve quality and lower the cost of providing care. |